Active vs Passive Immunity: Differences and Definition

Complete the form below to unlock access to ALL audio articles.
While the immune system incorporates all of the body’s defenses that help to protect us from anything that is not recognized as “self”, the term “immunity” is typically used to refer to the body’s ability to protect itself from infectious disease. If you are immune to a disease, it means your immune system is able to fight off infection by the causative agent.
Contents
- What type of immunity results from vaccination?
What is the difference between artificial passive immunity and natural passive immunity?
- Natural passive immunity
Immunity is made up of both innate and adaptive arms. Innate immunity, also known as natural or genetic immunity, is something an organism is born with, encoded in their genes and protects them throughout their life. Innate immunity consists of:
- External defenses: Known as the first line of defense, external defenses work to protect an organism from pathogen exposure and include things like the skin, tears and stomach acid.
- Internal defenses: Known as the second line of defense, internal defenses address a pathogen once it has entered the body and include things like inflammation and fevers and the chemical and cellular components that make up the innate immune system.
Innate immunity is fast to act but not specific to the potential threat.
Adaptive immunity, also known as acquired immunity, is the third line of defense and, whilst slower to act, protects an organism from specific pathogens. Adaptive immunity can be further classified into two subgroups: active immunity and passive immunity. In this article, we will explore active and passive immunity.
What is active immunity?
Active immunity is defined as immunity to a pathogen that occurs following exposure to all or part of that pathogen.
When the body is exposed to a novel disease agent, a cascade of signaling molecules and action from the innate immune system results in activation of the adaptive immune system. Production of large numbers of T cells and B cells specific to the pathogen are promoted. Subsets of T cells kill the pathogen directly while others help to stimulate B cell production. B cells, a type of white blood cell, produce antibodies that assist in destroying or neutralizing the disease agent. Antibodies are y-shaped proteins capable of binding to sites on toxins or pathogens called antigens.
Antibodies are specific to a particular antigen epitope, so depending on the similarity between pathogens, may or may not offer cross-protection between different diseases. For instance, antibodies produced when the body detects the virus that causes mumps will not provide any defense against measles or influenza viruses. However, antibodies generated to one strain of influenza, may offer some protection against other closely related influenza strains.
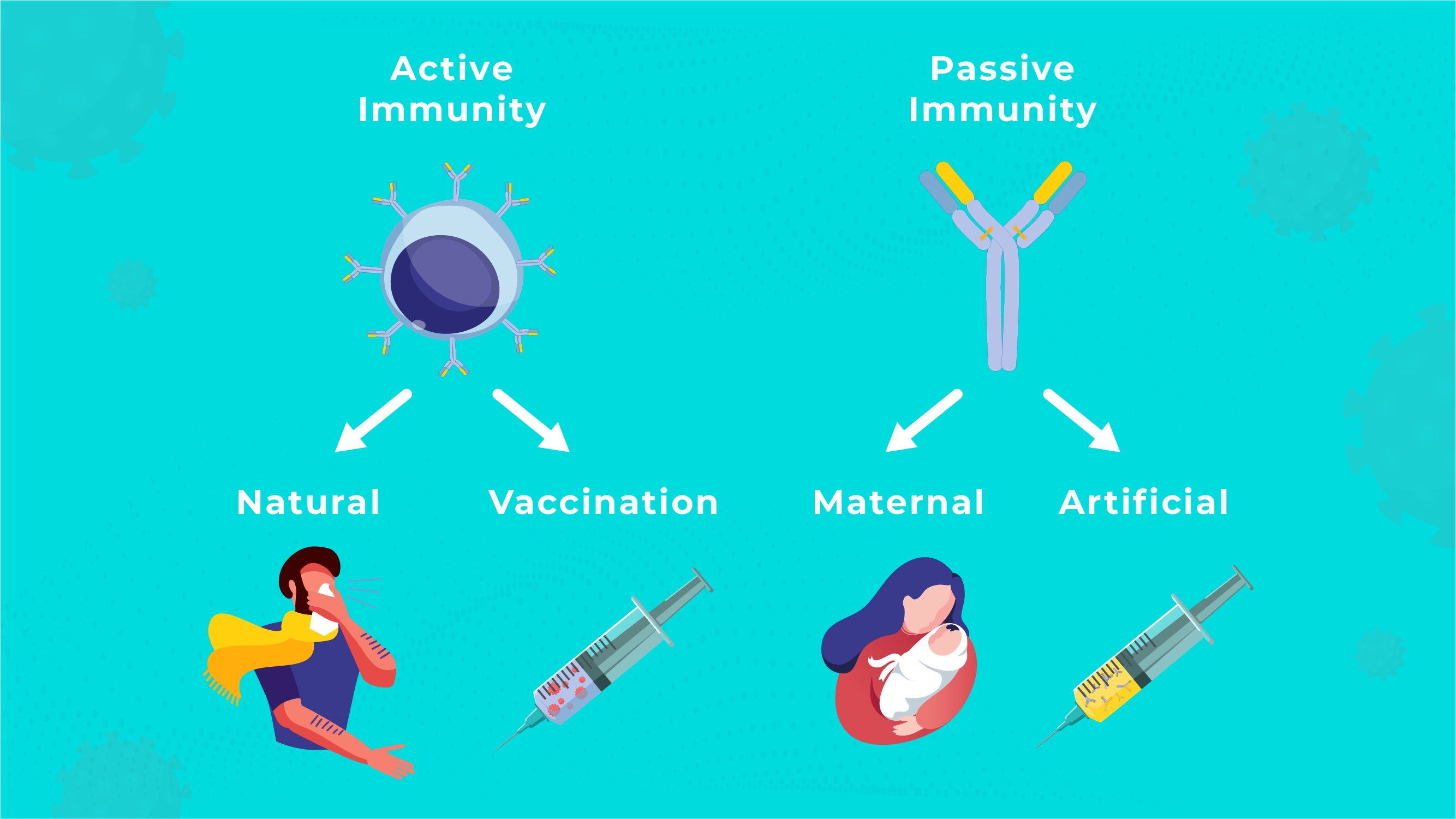
A diagram showing the different types of active and passive immunity. Credit: Technology Networks
Active immunity can occur in one of two ways: naturally or via vaccination.
Natural immunity
Natural immunity occurs when a person is infected by a pathogen. Take, for instance, someone who has chickenpox. After the initial infection, the body develops immune memory for the virus, conferring immunity against the disease so if they encounter it again, they are able to fight it off swiftly and don’t go on to develop clinical disease again.
Vaccine-induced immunity
Also known as artificial active immunity, a person can build resistance to a disease following an immunization. Immunization is the process that happens in the body following the administration of a vaccine aimed at conferring immunity to a pathogen.
Vaccines use a weakened or dead form of a pathogen or subunits from it that are known to stimulate the immune system to generate an immune response. Vaccines are typically administered using an injection, but some are also routinely administered via the mouth or as a nasal spray.
What type of immunity results from vaccination?
Vaccination produces active immunity. Vaccines introduce a killed or impaired version of a pathogen or a subunit of it into the body, giving our immune system a safe way to create an immune response. By using vaccination, an individual does not have to be exposed to a full-strength pathogen to generate an immune response.
When a person’s immune system detects the pathogen, it begins to take steps to destroy and remove it. This includes forming new antibodies and memory cells specific to that pathogen. In the future, if the body is exposed to the same pathogen again, the corresponding memory cells will become activated, stimulating the production of antibodies to protect the body. The main advantage of active immunity gained via vaccination over natural infection is that the individual doesn’t have to go through the disease itself to become immune.
Vaccination and immunity are essential for keeping large populations of people safe from infectious diseases. For instance, the influenza vaccine prevents millions of people from developing flu every year and the SARS-CoV-2 vaccination programs worldwide likely prevented vast numbers of cases and deaths.
What is passive immunity?
Passive immunity is protection from a disease provided by antibodies created outside of the individual’s body. Passive immunity:
- Does not require previous exposure to a disease agent (either through infection or vaccination)
- Takes effect immediately
- Normally does not last long (up to a few months)
Passive immunity is generally short-lived as the supply of antibodies is not being replenished as they would d be in someone whose own immune system was generating them.
What is the difference between artificial passive immunity and natural passive immunity?
Passive immunity can be either maternal or artificial.
Maternal passive immunity, or natural passive immunity, is immunity passed from mother to child. Whilst still in the womb, antibodies pass across the placenta to the unborn child and can confer protection against the corresponding infections in the weeks and months following birth. After birth, an infant continues to receive passive immunity to disease from antibodies found in breast milk, especially colostrum, the protein rich milk produced in the first few days following birth. Maternal passive immunity is important for protecting infants until their own immune system is mature enough to protect them.
Artificial passive immunity is conferred by the injection of antibodies generated by a different person or animal, or artificially in the laboratory, into an individual. These antibody-containing preparations are termed antisera and are used as a therapeutic treatment when there is a risk of some infections. Following a bite from a potentially rabies-infected animal, when a baby is born to a Hepatitis B-positive mother or following a bite from a venomous snake, the appropriate antisera or antivenom may be administered to offer passive immunity.
Natural passive immunity
Natural passive immunity is when a person receives antibodies to a pathogen that have not been generated by their own immune system by natural means rather than medical intervention. This typically refers to the passage of antibodies from mother to baby across the placenta so is also called maternal passive immunity.
Active vs passive immunity table
Active Immunity | Passive Immunity | |
Antibodies | Produced inside of the body | Introduced from outside of the body |
Results from |
|
|
Takes effect | Over time (typically weeks) | Immediately |
Length of efficacy | Long-term to lifelong | Short-term |
Generates memory cells? | Yes | No |






